
The heart is an amazing muscle that is located in the chest cavity. In a healthy adult it is about the size of a fist and pumps blood around our bodies – beating around 100,000 times a day.
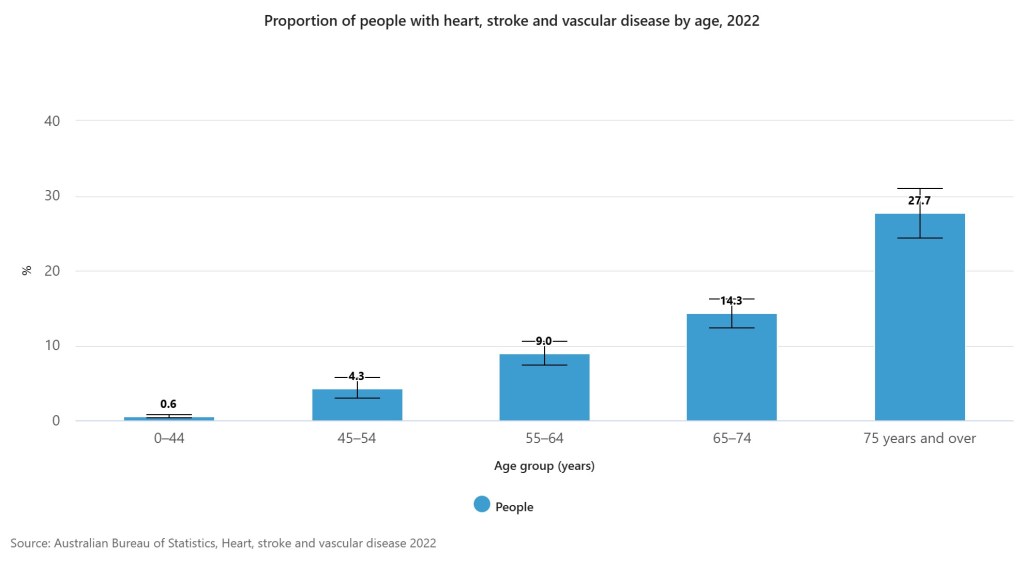
Molecular damage contributes to the process of ageing and the development and/or progression of cardiovascular disease (CVD). This is reflected in 2022 statistic from the Australia Bureau of Statistics, the risk of developing CVD increases with age (see table below) and is slightly more common in men (5.9%) than women (4.6%). In 2022 CVD affected 1 in 20 (or around 1.3 million) people, with 90% of all heart failure deaths occurring in individuals aged 70 years or more.
Ageing itself is not a cause of CVD, however, the changes that occur to us as we age increases the risk of CVD. There are several changes that occur with our cardiovascular system as we age, such as structural and functional changes, changes to the body’s ability to protect and repair itself and the impact of other diseases and/or conditions within the body (comorbidities).
These changes are not limited to, but can, include the buildup of fatty deposits (plaque) in the walls of our arteries and vascular stiffening, the hardening of arteries (arteriosclerosis), and high blood pressure (hypertension).
Other changes include the reduced ability of the heart to respond to increased workload and decreased reserve capacity, such as during physical activity or times of stress. As the systems of the body age, the mechanisms that protect and repair our bodies from injury become less efficient and/or defective.
Other risk factors of developing CVD include where we live. In Australia, living in a more disadvantaged area, living in Inner Regional Australia and/or living with a disability increases the risk of developing CVD according to the Australia Bureau of Statistics (2022).
Additional lifestyle risk factors include increased weight, smoking, and/or having experienced severe or very severe pain in the last 4 weeks.
Ways to help reduce the risk CVD?
One thing we can do is to contain other risk factors or pre-existing conditions such as diabetes, blood pressure, obesity, cholesterol levels and stress. Other proactive lifestyle choices we can make includes remaining physically active, and aiming for 150 minutes of exercise every week (or 30 minutes 5 days a week)! We can achieve this by everyday activities and avoiding sitting for prolonged periods of time every day.
Smoking is damaging to the artery walls therefore, stopping smoking can lower your risk of developing CVD among other health benefits.
We can also make dietary choices to help reduce the risk of developing CVD. Such as choosing foods low in saturated fats, added sugars and salt. Instead, we should try to eat a wide variety of vegetables, fruits, and nuts (try to eat the rainbow).


Foods that may promote heart health include those high in vitamin B6 (Fish, leafy greens, bananas), folic acid (leafy greens, asparagus, legumes, nuts), vitamin C (oranges, rockmelon, broccoli, tomatoes), vitamin E (wheat germ, avocado, eggs, oily fish), and Omega 3 (oily fish, oysters, linseed, walnuts).
Herbal remedies such as Hawthorn, Andrographis, and Rosemary can also help heart health.


Subscribe for access to more articles on health, herbs, nutrients, and recipes! Next month we will continue to explore 5 Common Health Complaints of Ageing as we explore Diabetes.
If you have any questions, concerns, or would like a personalised health plan contact us for your individualised consultation today!
Resources
Booth LK, R. R. T.-C. S. S. I. P. H. R. G., 2023. Heart Disease and Ageing: The Roles of Senescence, Mitochondria, and Telomerase in Cardiovascular Disease.. Subcell Biochem, Volume 103, pp. 45-78.
Shaffer, F., McCraty, R. & L., Z. C., 2014. A healthy heart is not a metronome: an integrative review of the heart’s anatomy and heart rate variability. frontiers in psychology, Volume 5.
Strait, J. B. & Lakatta, E. G., 2012. Aging-associated cardiovascular changes and their relationship to heart failure. Heart Failure Clinics, 8(1), pp. 143-164.
Leave a comment